Is topical steroid withdrawal real?
Topical steroids - the wonder drug of the 1950s
Topical steroids, also known as cortisone, TCS, and steroid creams, were introduced as a new ‘wonder drug’ for eczema back in 1952. However, since then the incidence of eczema has more than tripled.
Topical steroids are often recommended by medical professionals as they can temporarily suppress the symptoms. However, the overuse can lead to chronic eczema that is more severe than the original symptoms — it’s known as topical steroid withdrawal or topical steroid addiction.
Is TSW real?
Yes! Topical steroid withdrawal may seem like a new phenomenon and some doctors question whether the condition even exists. However, topical steroid addiction was identified back in the 1970s, according to a study called ‘Steroid addiction’ published in the International Journal of Dermatology in 1979.
The revealing paper detailed how frequent topical steroid use caused stunted growth in children, Cushing’s syndrome, severe eczema and one fatality. A child with psoriasis died after the mother compulsively applied strong topical steroids and the child died of adrenal failure after the mother suddenly stopping using the steroid creams. Do not be alarmed, this happened a long time ago and warnings are now in place to prevent fatalities from happening.1 Note it's best to stop using the steroids creams by gradually cutting down on use. I have helped hundreds of eczema and TSW sufferers and I will describe the steps I use to LIMIT the side-effects of TSW later in the article.
Topical steroid side effects list
Side effects from frequent use of topical steroids are well established. Warnings from the manufacturers appear on the packaging in fine print, including ‘Do not use on broken skin’ (eczema is broken skin!) and ‘Do not use for more than 7 days’. While not everyone will experience side effects, this is what can occur with long-term topical steroid use.
Side effects of excess topical steroid use include:2,3,4
- red skin syndrome
- stubborn, eczema-like rashes
- red, burning skin
- raw, painful skin
- swollen, oozing skin
- deeply crevised/wrinkled skin on arms and legs
- purplish streaks on skin
- scar-like lesions
- adrenal suppression
- skin thinning (common)
- skin depigmentation
- dark pigmentation
- Cushing’s Syndrome
- broken blood vessels
- leg ulcers
- mouth dermatitis
- steroid acne
- rosacea-like dermatitis (red skin)
- transformation to pustular psoriasis
- stunted growth in children
- excess nitric oxide (widens blood vessels)
- difficulty regulating body temperature
- hair loss/thinning hair
- loss of eyebrows
- adverse reactions to all skin care products
- fatigue
- sleep problems
- fatty liver disease (non-alcoholic fatty liver)
Many symptoms are worse than the original eczema or psoriasis.
Fatty liver disease
Frequent use of topical steroids can cause fatty liver and other liver injuries according to the United States National Library of Medicine.7 Fatty deposits in the liver can hamper the liver’s detoxification ability and have been liked to the appearance of eczema.8
Fatty liver can be diagnosed via ultrasound. It can take more than three months to reverse fatty liver. To help reverse fatty liver follow the Eczema Detox Program (or the eczema diet) and take Skin Friend AM.
What happens to your body when you use topical steroids?
Topical steroids constrict blood vessels and this usually prevents skin reddening. Topical steroids can also temporarily suppress skin inflammation and reduce itching so your skin appears clear.
That sounds great. However, eventually the creams stop working and you need higher doses, applied more frequently.
This is why you should NOT suddenly stop using topical steroids
If you keep applying the creams daily for expended periods (some people use the creams on and off for years) and then you decide to suddenly stop applying topical steroids, a crazy chemical imbalance occurs. Your blood vessels excessively dilate due to high nitric oxide levels (see diagram below).
Within a week your skin appears redder and itchier than previously.
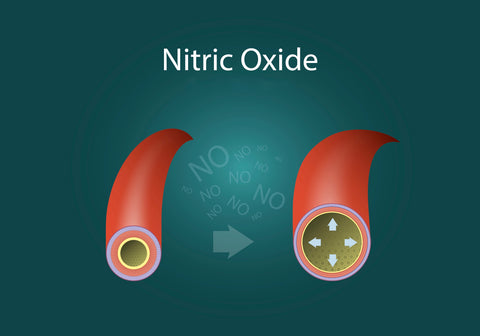
Diagram 1: the left blood vessel is normal, and the right blood vessel is excessively wide from elevated nitric oxide in the blood.
This can cause skin flushing and red skin, hence the name ‘red skin syndrome’.
Since the red skin syndrome (TSW) recovery phase can take more than a year, a person’s nitric oxide levels can be measured to gauge how long it might take them to recover from TSW and for their skin to calm down.5
Next steps
If you suspect you are suffering from TSW/red skin syndrome begin on the Eczema Detox Program (or The Eczema Diet) to boost your nutrient intake for at least twelve weeks or until your skin has recovered. You can read some accounts of people who have used these programs to help their TSW here.
Do not do this alone. There is support out there for TSW sufferers and organisations such as itsan.org.
Key point to remember
- If you are using topical steroids, wean yourself off them slowly - very gradually in order to minimise damage. Read the article 'How to avoid or limit TSW' here >>
Products
At Eczema Life, we recommend nutritionist Karen Fischer's low food chemical program (The Eczema Detox) along with additive-free supplements for skin health and wellbeing. Click on the images to view more details:
Supporting research
- Kligman, A.M. and Frosch, P.J., 1979. Steroid addiction. International Journal of Dermatology, vol.18, no.1, pp.23-31.
- ibid.
- ITSAN Red Skin Syndrome Support, ‘Coping with RSS’, retrieved 1 November 2016 from http://itsan.org
- Rathi, S.K. and Kumrah, L., 2011. Topical corticosteroid-induced rosacea-like dermatitis: A clinical study of 110 cases. Indian Journal of Dermatology, Venereology, and Leprology, 77(1), p.42.
- Rapaport, M.J. and Rapaport, V.H., 2004. Serum Nitric Oxide Levels in Red Patients: Separating Corticosteroid-Addicted Patients From Those With Chronic Eczema. Archives of dermatology, 140(8), pp.1013-1014.
- Chiang, T.T., et.al., 2013. Recreational nitrous oxide abuse-induced vitamin B12 deficiency in a patient presenting with hyperpigmentation of the skin. Case reports in dermatology, 5(2), pp.186-191.
- United States National Library of Medicine, Drug Record: Corticosteroids, LiverTox, retrieved from: https://livertox.nih.gov/Corticosteroids.htm
- Kimata, H., 2005, ‘Prevalence of fatty liver in non-obese Japanese children with atopic dermatitis’, Indian Pediatrics, vol. 42, no. 6, p.587.